The mouth falls victim to numerous types of aches and pains throughout our lifetimes. With 32 teeth functioning almost continuously throughout the day, there’s a lot that can happen. If you are having a toothache, gum pain, or potentially a dental abscess, you are probably wondering how to stop a toothache, and what’s causing it. In this article, we’ll explore the most common causes of toothache, teeth sensitivity, and dental abscess.
Tooth Pain Has Different Causes
Tooth pain is one of the most diverse pains in the body. It may be caused by several types of irritants, all of which are felt in the same part of the tooth, the dental pulp.
The dental pulp is probably something you never considered, but it is where the majority of tooth pain is felt. The dental pulp runs the length of the tooth. It is the only area of the tooth that contains a nerve.
When it comes to pain, think of the outer enamel of the tooth like a helmet, protecting the inner nerve. The whole goal of the enamel is to provide a buffer from irritation. When the helmet of the tooth is pierced, either by bacteria, a fracture, pressure, or wear… the nerve recognizes the potential for damage. The tooth warns us by sending the sensation of pain.
When Should I See a Dentist for Tooth Pain?
Although a one size solution doesn’t always fit everyone, there is a good rule of thumb. If you have mild pain for over a week, or if you have moderate/severe pain for over 48 hours, it is a good idea to discuss with your dentist. However, there is one caveat, if your tooth pain is associated with swelling, a fever, or an injury from an accident, you should contact your dentist immediately.
The Most Common Causes of Toothaches
Tooth Decay
Decay is what lay people refer to as a cavity. Dental decay affects 9 out of 10 people over the age of 20. To put it into perspective, cavities are 4x more common than asthma. The prevalence is universal across the globe.
The reason cavities are so common because bacteria naturally live in all humans mouths. The bacteria use sugar in our diets to produce an acid which creates holes in the teeth. We call the holes, dental decay or cavities.
The bacteria work progressively. Once a cavity has started, the bacteria continue to tunnel deeper into the tooth. As the depth increases, we begin to feel sensitivity until the cavity reaches a tipping point. The tipping point occurs when the bacteria reach the dental pulp and an infection occurs.
The first symptom of dental decay is often sensitivity when drinking cold water which worsens over months or even years. The goal for treating dental decay is to act before the bacteria progress deep into the tooth. A tooth which is treated early may be corrected with a simple composite filling, which effectively removes the decayed portion of the tooth and restores it. When decay is more advanced, more tooth structure is affected. A dentist corrects a tooth with a large amount of decay by sealing it with a dental crown.
Tooth Abscess
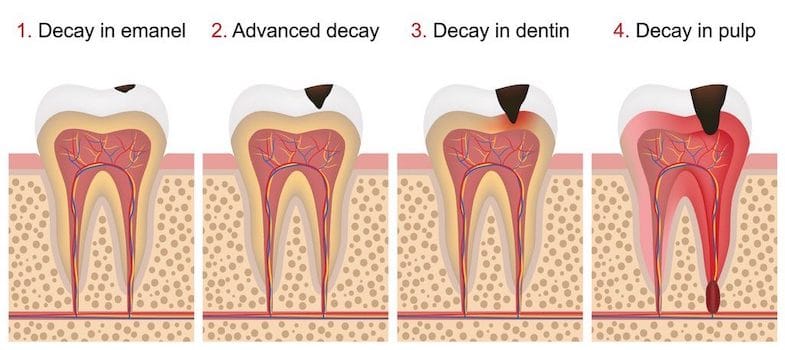
When dental decay progresses a long time, it eventually tunnels all the way to the dental pulp. Once bacteria reach the pulp, the nerve and blood supply of the tooth are exposed to bacteria, which cause an infection. A tooth infection is called a tooth abscess.
The interesting thing about teeth, compared to the rest of the body, is they are a closed space. The bacteria enter through the cavity and have nowhere else to go except down the root. A tooth abscess is the body’s way of shuttling the pressure of infection out of the tooth. It usually forms at the end of the root and causes swelling of the bone and gum in that area, eventually creating a bubble under the gums.
The symptoms of an dental abscess are pulsing and throbbing sensations that have swelling at the gumline. The gums usually feel tender and warm to the touch.
A tooth absess means that the root of the tooth is compromised. To treat a dental abscess, a dentist will recommend a root canal and crown, or if the abscess is severe enough, the dentist may recommend to extract the tooth in preparation for a dental implant.
Cracked tooth
A cracked tooth is a matter of physics. When forces on the tooth exceed the amount of strength of the tooth structure, a fracture can occur.
Cracked teeth are more common in teeth that have large fillings. Large fillings create seams on the teeth which act as fault lines. In addition, the shape of teeth affects the probability of fracture. Teeth that have steep inclines of the cusps, as opposed to flat teeth, are more likely to crack. The sharp cusps create leverage of force which leads to higher probability of cracked teeth.
The symptoms of a cracked tooth are usually sensitivity when biting on the tooth. Sometimes the tooth may have a hairline crack, and other times a cusp or even the entire crown of the tooth can break off. Symptoms generally will increase along with the severity of the fracture. The exception is when a tooth has been root canal treated previously. A root canal treated tooth will not feel pain when a fracture occurs.
Many cracked teeth can be restored with a dental crown, but in some circumstances a root canal, or even a tooth extraction may be needed if the tooth is deeply damaged.
Sensitivity After Recent filling
When patients have fillings completed, it is common for the tooth to be sensitive to cold for several weeks or even a few months afterwards. It doesn’t happen every time, but it is relatively common.
When a tooth has a filling, it must be opened and cleaned out to allow it to heal. When the tooth has sensitivity after a filling, your body is telling you that the tooth is healing, similar to a bruise. Many dentists now use a desensitizer, which is a medication placed under the filling that usually avoids this complication.
If your tooth is sensitive after having fillings done, you should discuss it with your dentist. Sensitivity may often recover with time, or it may be a simple correction of adjusting the bite of the tooth. In some cases, a toothache may become increasingly sensitive after a deep filling and your dentist may recommend a root canal.
Teeth Grinding and Teeth Clenching
Teeth grinding is a common symptom of TMJ dysfunction, a disorder that affects up to 70% of humans worldwide. Teeth grinding is both a habit, and also a sign that the jaws aren’t in ideal harmony.
The thing with teeth grinding is that it can progress. Although it might seem like a simple annoyance, teeth grinding can be linked to cause many conditions such as tension headaches, muscle pain, jaw popping, knotching on the sides of the teeth, and even ear ringing.
The best thing to do is to discuss it with your dentist. Because teeth grinding can be part of the more complex TMJ disorder, your dentist may refer you to a TMJ specialist.
Common treatments for teeth grinding/clenching are orthodontics, balancing the bite, botox, and restoring broken teeth. All these treatments serve to provide better harmony of the top and bottom jaw. Better harmony creates a more stable home for the jaw to site without grinding.
Sinus Infection
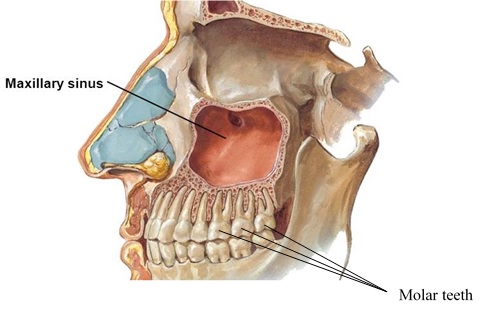
The sinus and the top back teeth have a close association. For many people, the roots of the top teeth are actually half in the sinus.
When a person has sinus pressure, it is common for them to have a toothache. Many patients go to their dentists with tooth pain which seems to affect normal teeth. When the dentist is unable to find a cause of tooth pain on the top back teeth, it is always best to think of the sinus.
If the patient recently had a cold, seasonal allergies, or feels pressure in their sinus when leaning over, you can bet its the sinus putting pressure on the roots of the teeth. If there are no other signs of dental problems, its best to watch the tooth for improvement over the next couple weeks, often with the help of an antibiotic or an antiallergy medication to assist.
How long does a sinus toothache last, typically it should return to normal in 2-3 weeks. If the toothache doesn’t improve, you should refollowup with your dentist.
Wisdom Tooth Pain
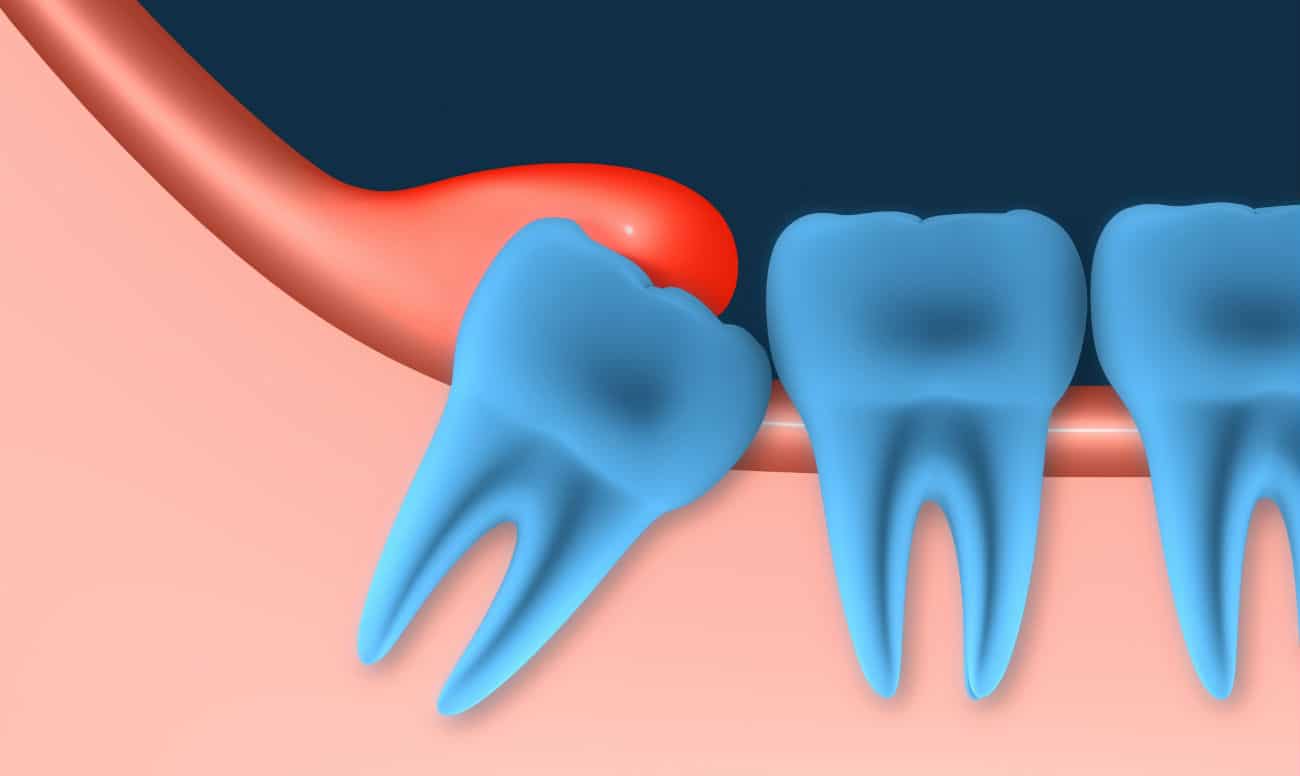
The wisdom teeth are the last teeth to erupt in our mouth, but for many people they are the first and hopefully only teeth needed to be extracted. Wisdom teeth are common causes of toothache, but also jaw pain and even ear pain. The reason is because most wisdom teeth lack space. The wisdom tooth tries to erupts but usually pushes against the back off the tooth in front of it. The result is pain. Even whena wisdom tooth does erupt there are often problems. The wisdom teeth are difficult to clean and are often at angles which create flaps of gum tissue that easily become infected.
Pain from a wisdom tooth feels like a general ache at the back of the mouth which often radiates to the jaw or ear. The wisdom tooth may have swelling or may have pain without swelling. Limited mouth opening is also a symptom that often occurs together with wisdom tooth pain, particularly with the lower wisdom teeth.
A dentist or oral surgeon, will evaluate the wisdom teeth and generally will recommend to extract the wisdom teeth. After healing, the pain from wisdom teeth completely resolves within 2-3 weeks.
Infected Gums and Periodontitis
Infection of the gums happens when bacteria collect around the gums or when foreign objects become caught. The most noticeable symptoms are an aching sensation of the gum between the teeth and bleeding when flossing.
The treatment most often recommended is a deep cleaning of the area which is also called scaling and root planing. During scaling and root planning the dentist numbs the gums of the teeth and cleans below the gumline to remove the irritants and bacteria. The gum sensitivity typically resolves in 2-3 days after a deep cleaning.
Receding gums
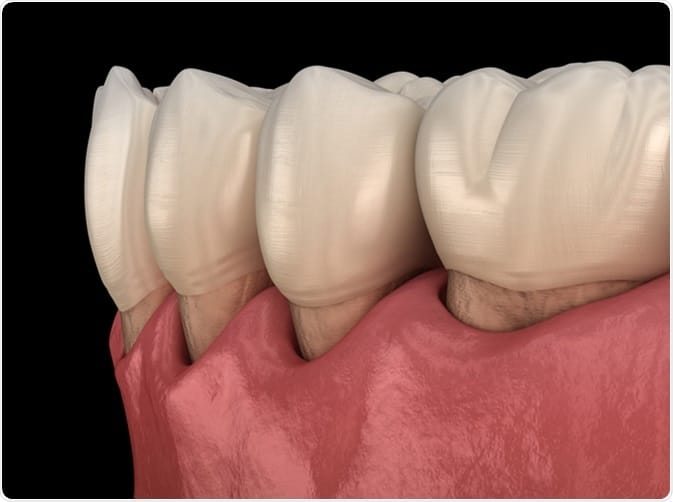
Sensitivity from receding gums is like going outside on a winter day without a coat. As the gums recede, it exposes the underlying root of the tooth. The root of the tooth is not covered by enamel like the crown of the tooth is. It provides less protection.
People with receding gums will feel a zing sensation when drinking cold drinks that lingers for a few seconds.
Receding gums are most often corrected by a gum graft. You may have also heard of gum grafts referred to as connective tissue grafts in technical jargon. The gum graft covers the root of the teeth which not only reinforces the tooth, but also protects it from feeling sensitivity from cold or touch.
Dentin hypersensitivity
Dentist hypersensitivity is probably one of the dental terms you haven’t heard of, but its actually a pretty simple concept. The sensitivity after teeth whitening is most commonly associated with dentin hypersensitivity.
Did you know that teeth have pores similar to the skin? In the case of the tooth, they are called dentin tubules. What happens when we whiten our teeth is the gel opens the tubules and cleans them out. During the process, it leaves the pores of the teeth temporaily open to fluids and air. The teeth have a temporary phase of toothache that feels like a spontaneous electrical sensation that lasts for a few seconds.
The sensitvity from dentin hypersensitivity has no long term effects on the teeth and typically the resolves in 3-5 days. To cope after whitening, you can manage teeth sensitivity with a toothpaste designed for sensitive teeth in the meantime.
We Will All Have a Toothache at Some Point
After reviewing all the things that can ruin your day with a toothache, the best advice I can give for long term success is prevention. By routinely seeing your dentist for checkups and dental cleaning, you are giving yourself the best opportunity to avoid many of the above problems. And, with that, I’d like to leave you with a quote about prevention:
“A good doctor cures the disease, but a great doctor cures the cause.”
― Amit Kalantri, Wealth of Words