When’s the last time you thought about your gums? Well, fortunately, probably not, unless your gums are unhealthy from periodontitis, or your gums are the source of self-consciousness from a gummy smile.
From a mental health standpoint, that’s probably a good thing. It would be bordering on a disorder if you obsessed about your gums all day long.
But maybe we should think about our gums a little more, at least that’s what the studies now show. I’d like to share with you the hard facts about gum disease, why it matters, and why new research is showing us that longterm problems with the gums from periodontitis can be down-right scary.
What is Periodontitis
For some mysterious reason, most people have an aversion to flossing. Brushing without routine flossing is like washing your hair, but not your face. You’re missing a surface. So if you were to ask me for a cheeky answer to what is periodontitis, I’d say: Periodontitis is punishment for not flossing. That’s partly true, but sadly… gum disease is much more than that.
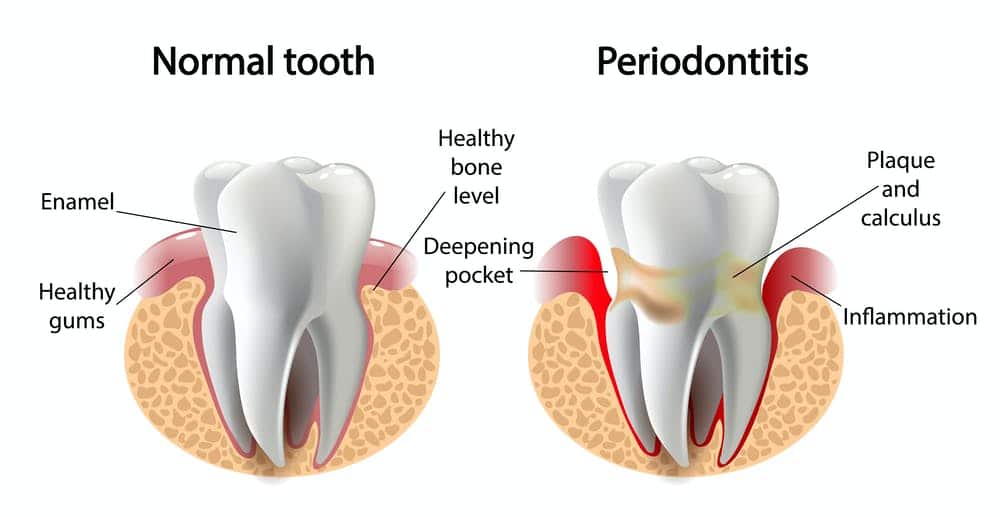
Periodontal disease is a long-term infection. The gums become inflamed from bacteria that collect around the teeth and under the gums. Eventually the gums develop pockets around the teeth due to deterioration of the bone.
And you’ve probably heard that periodontitis takes years to develop, which is true. So what’s the big deal? Here’s the bottomline: Periodontitis is a slow-burning fire that has massive consequences over time.
The reason periodontitis shouldn’t be ignored is that it affects much more than just the gums. It affects the jawbone, which can cause loss of teeth, it can create an unsightly appearance of the gums, an odor, and now new research is showing some pretty startling links to damage to our neurological health (more on that later).
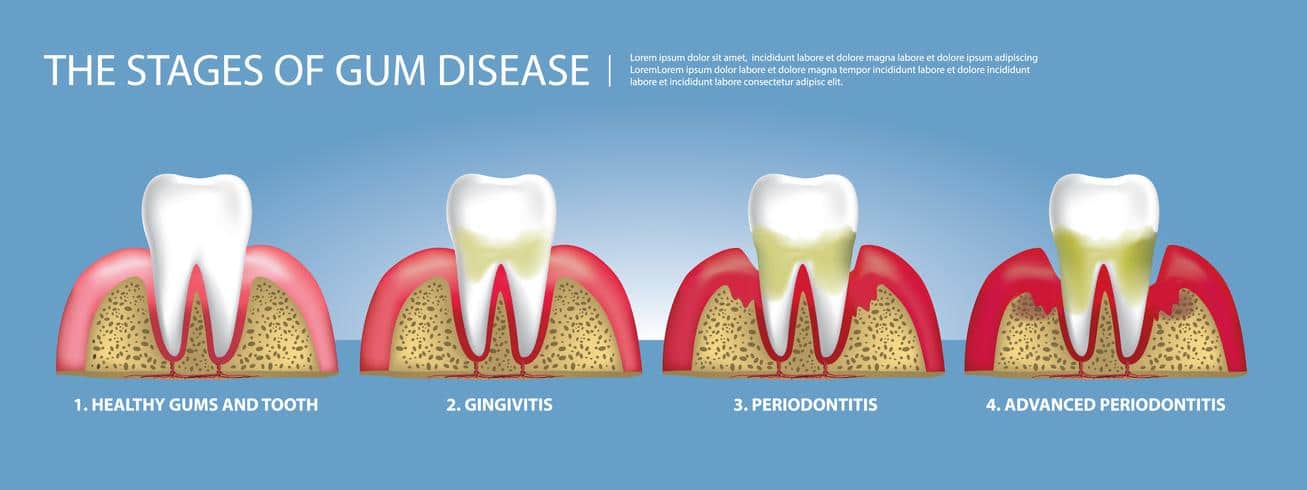
Periodontitis progresses slowly over time in four stages. One of those stages is reversible, but the other stages all cause loss of bone and gum that is often difficult to fully regenerate.
The four stages of gum disease are gingivitis, slight periodontitis, moderate periodontitis, and severe periodontitis. Each state generally indicates the amount of bone and gum lost at that point, with gingivitis being the only stage where there are signs of inflammation and now damage yet. All four stages can be treated and arrested at that point for further destruction, but it is difficult to regenerate the bone lost as phases become more advanced.
What are the Signs of Periodontitis
If you’re looking in the mirror and wondering if you should see a dentist or gum specialist for periodontitis, here’s what periodontitis looks like:
- Red, swollen or tender gums
- Sensitivity or pain when chewing
- Bleeding while brushing or flossing
- Persistent bad breath or taste
- Receding gums or teeth appearing longer than before
- Changes in the way teeth fit together when biting, known as occlusion
- Loose teeth and loss of teeth!
What Causes Periodontal Disease and How do I Prevent it?

A vector illustration of germs attacking teeth causing cavity
When it comes to periodontitis, it’s all about bacteria. The amount of bacteria, location, length of time under the gums, and even the quality of bacteria in the mouth…all affect severity of gum disease. Wait, did I just say quality of bacteria? What does that mean?
Well, when most people think of an infection, they know that its caused by bacteria. That’s true, but there’s different types of bacteria, and some are more benign than others.
If you’ve heard the terms staph infection, strep, or MRSA, you’re already familiar. Those are all types of bacteria. Each type of bacteria not only affects the body differently but needs to be treated differently.
Here’s what you need to know about the bacteria of the mouth. The bacteria are either aerobic (they need oxygen to survive) and anaerobic (they can survive without oxygen). The anaerobic bacteria are significantly more destructive to the bone and gums. And if they don’t need oxygen, where do you think they live best? Under the gums.
So not only are anaerobic bacteria more destructive, they are capable of living in places that are difficult to clean. That’s a recipe for disaster. That’s how bacteria destroy our mouths by way of periodontitis.
Can I Catch Periodontitis? Gum disease is Partly Genetic, Partly Not
Here’s what you need to know about how periodontitis develops. Periodontitis is the product of three factors, two of which are controllable and one which is not. The three factors are hygiene, lifestyle, and genetics.
Hygiene
First up is hygiene. If plaque and tartar are not regularly removed (using good daily flossing and brushing habits, as well as regular professional teeth cleanings), bacteria is likely to build up and periodontal disease will occur. It’s like if you never washed your hands or trimmed your fingernails, eventually bacteria would buildup under the nail bed. The nails would collect crud that cannot easily be washed out, and infection would arise. The same concept applies to the mouth. Consistent oral hygiene is needed to prevent bacteria from getting caught under the gums.
Lifestyle
Next up is lifestyle. Certain lifestyle factors increase the risk of periodontitis. These lifestyle factors all create an environment in the mouth where a greater quantity of the bad anaerobic bacteria can exist. The big one is smoking. Smoking significantly increases your risk for periodontal disease but that’s not all. It hits you with a double whammy. Smoking also reduces the effectiveness of periodontal treatment and the success of procedures like dental implants. Other factors that increase one’s risk for periodontal disease include medications, alcohol, or drugs that reduce saliva flow, diabetes, hormonal changes, and dehydration.
Genetics
The final factor that affects who develops periodontitis is genetics. Yes, we all naturally have bacteria in our mouths. In fact, a healthy level of bacteria is good for the balance of our immune system and digestive system. However, some people have a higher ratio of the bad anaerobic bacteria compared to the aerobic bacteria. Its just the way genetics work out sometimes. Periodontitis is also genetically linked to culture. Studies show that periodontitis is more common in Asian cultures compared to the average population.
Now, I have to reiterate that two of the risk factors for periodontitis are controllable, and one is not. Obviously, we can’t control our genetics, but the genetic factors are not a death sentence in terms of periodontitis.
You can overcome the genetic risk factors for periodontitis by increasing oral hygiene and decreasing lifestyle factors that contribute to gum disease.
How Long does Periodontitis Last
What it all comes down to is…how long does periodontitis last and how is it treated. That’s a bit misleading the way I phrased that because its two very separate things. The progression of periodontitis stops as soon as the bacteria is removed that is causing inflammation. However, the bone loss and gum loss caused by periodontitis is a separate issue. Sometimes bone and gum can be regained by grafting, but there is a certain percentage, particularly in advanced cases, that cannot ever be regenerated.
So how do we arrest periodontitis and rebuild? It’s simple. It’s similar to how a town would rebuild after a natural disaster. The destructive agent is removed, in this case, the bacteria. The bacteria are manually removed by cleaning below the gumline with tools during a procedure known as scaling and root planning. Then the patient must commit to maintaining a healthy environment consistently by proper home hygiene and professional cleanings periodically.
The inflammation from periodontal disease actually reduces fairly quickly in the first weeks or months after the bacteria is removed. Once the inflammation is gone, the teeth can be reinforced with bone or gum grafting, or replaced with dental implants. That’s how you stabilize and rebuild after gum disease.
Where the Periodontitis Story Gets Kind of Scary
Have you ever watched a movie where the first half is pretty boring but then the story starts to unfold. Suddenly you’re on the edge of your seat, clutching the armrests, as the story takes you on a roller coaster ride of new details. That’s what periodontitis is for me.
At first glance, the topic of periodontitis seems pretty dry. It’s an inflammation of the gums, and yes, its tragic to loose teeth from it, but ultimately not a thriller of a topic. But then a few years ago new research started to hit. I was floored. Study after study, research on periodontitis started pouring in a little over a decade ago. It became clear that there was much more to periodontitis. And, it’s baffling. Allow me to explain.
Periodontitis has far more dangerous possibilities than just bleeding gums and losing teeth. Try wrapping your mind around that researchers have linked periodontitis to cardiovascular disease, Parkinson’s disease, and Alzheimer’s disease. How could the gums be linked to cause of such devastating diseases. As I said, I was floored when that research first came out, but it’s the reality.
Here’s what the most current research is now showing. In a 2017 study researchers found that periodontal disease was linked with increased likelihood of patients developing parkingson’s disease, and then in 2018 a study showed that dental scaling decreases the risk of parkinson’s disease.
In 2019, a study showed that patients with Alzheimer’s disease had periodontal bacteria in the brains. The researchers noted a link between periodontitis and Alzheimer’s disease, and postulate that by decreasing bacteria in the brain can help treat the disease.
Where We are Going with Periodontitis
Let’s put it all into perspective. Periodontitis is a largely preventable human condition, so why wouldn’t you prevent it? There’s clearly significant dental implications to periodontitis, but new research is showing that there’s overall health impact that is potentially very scary.
As new research develops, the picture will become more apparent, but it is promising to see we are now developing an understanding how inflammation in one part of the body can have both positive and negative effects to overall health. By developing this understanding, it will undoubtedly help improve overall healthcare and treatment of a vast amounts of conditions.


