When people have unrelenting jaw pain, clicking, and popping there are a million things that go through your mind. But of course, your primary thought is… what can I do to rid myself of this discomfort? So you start searching for TMJ treatment. And then reality sets in and you freeze. Well, what if my TMJ pain is serious? And worse yet, what if it requires TMJ surgery?
These are normal fears that everyone with debilitating TMJ pain begin to wonder about. Despite how bad TMJ pain may be, no one wants surgery. It’s something most people dread. And rightfully so.
But the good news is that the majority of people (more than 99%) won’t require surgery to successfully treat TMJ disorder. Phew! Yes you can breathe a sigh of relief.
In this article, we’ll talk about TMJ surgery. I’ll answer what do they do for TMJ surgery, when it’s needed, the success rate, and TMJ surgery risks.
Can TMJ surgery Help?
Here’s the thing about TMJ disorder. The name misleads us.
Because TMJ disorder is named after the temporomandibular joint (TMJ), it leads most people to think that the majority of the problem is from the TMJ. However, that’s not necessarily the case.
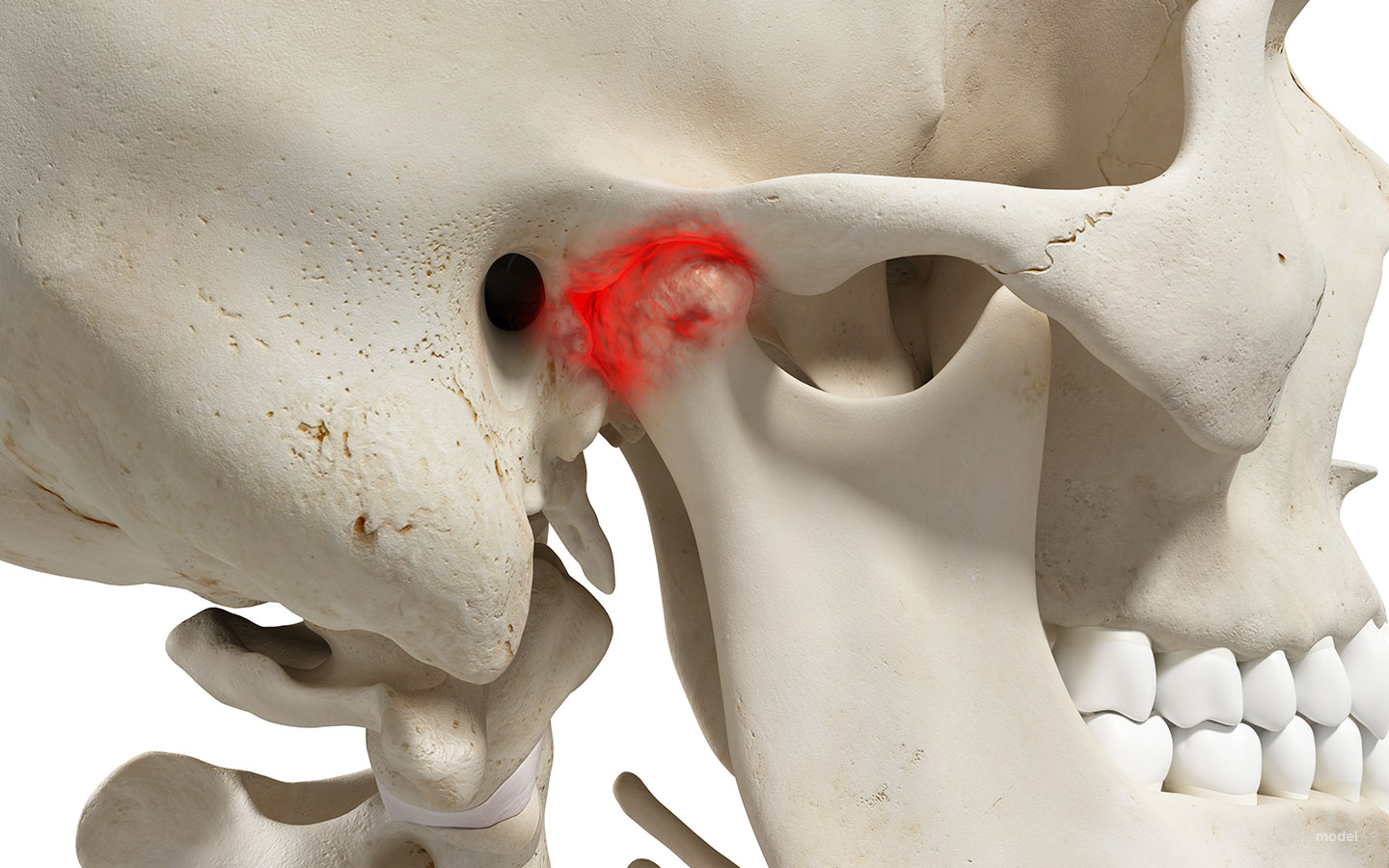
The TMJ is a hinge-like joint located where your jawbone and skull meet. The TMJ allows your jaw to open and close. It’s the joint responsible for allowing you to talk, eat, laugh, clench, and everything else your mouth does during the day.
And although the TMJ is the namesake of TMJ disorder, it’s not responsible for the majority of the symptoms. The reality is that symptoms of TMJ disorder can be from many things. The muscles, the ligaments, the nerves, and the alignment of the jaws all play a factor. So although TMJ disorder is named after the temporomandibular joints, the TMJ is the least likely to be the primary problem.
But that’s a good thing. Because the TMJs are located within the sides of the head. They are difficult to access. However, they can be adjusted indirectly by treating issues with the muscles, ligaments, jaw, and teeth that are associated with them. Modern TMJ treatment attempts to indirectly treat the TMJ first, before opting for invasive surgery. And luckily it works in the majority of cases.
Surgery may be used to treat a TMJ disorder if more conservative treatments prove to be ineffective. Typically a TMJ specialist will treat TMJ disorder with oral splints, orthodontics, bite adjustments, or botox before considering TMJ surgery.
For only a select few people, approximately 1%, TMJ surgery may be best.
When is TMJ surgery needed?
As I mentioned, it’s not needed in the majority of cases, but there are some times when TMJ surgery may be the best option.
Your general dentist is a good place to start the discussion of TMJ issues, however, you should know that most general dentists are not specialists of TMJ disorder. It’s important to be evaluated by a dentist, TMJ specialist, or physician who’s trained in TMJ dysfunction.
The specialist will perform a detailed examination of your history, your lifestyle, your head and neck, your teeth, and your radiological findings to determine the best course of treatment.
Your doctor may recommend TMJ surgery if:
- You have structural issues or diseases of your jaw joint which is confirmed by imaging such as MRI
- You have tried numerous more conservative TMJ treatments and your symptoms have not improved
- Your jaw alignment is so significantly out of alignment that the teeth cannot be properly aligned even with braces or orthodontics.
- You have tried medication, physical therapy, chiropractic, or lifestyle changes and there is no effect on symptoms.
What do they do for TMJ Surgery
There are a few different types of TMJ surgery which are selected based on symptoms and the underlying causes. I want you to think of TMJ surgery in two categories: 1) surgeries of the TMJs and 2) surgeries of the jaw. Let’s talk about some of the types of TMJ surgery.
Surgeries of the TMJs
Arthrocentesis
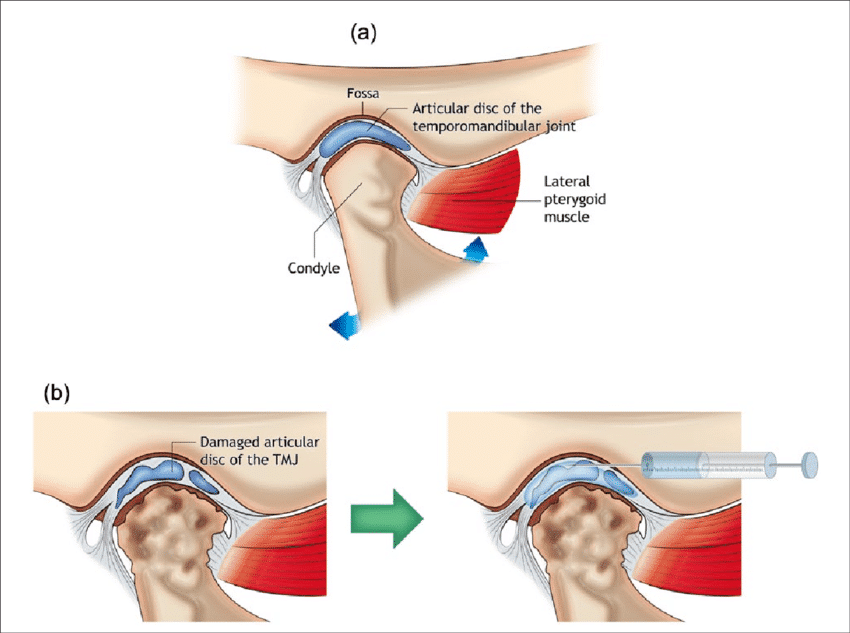
This is the least invasive type of TMJ surgery. There are not any incisions or stitches needed for this procedure. Think of arthrocentesis like getting an oil change in the car. Sometimes a little lubricant goes a long way. Arthrocentesis involves inserting needles to inject a fluid that lubricates the joint and reduces friction.
Arthroscopy
Arthroscopy is a minimally invasive procedure, but usually requires a small incision on the side of the area of the TMJ. A scope is used to look at your joint and then small tools are used through a cannula that removes scar tissue, smoothes the bone, or adjusts the position of the articular disc of the TMJ.
Arthrotomy or Arthroplasty
These procedures are a bit different because they are more invasive than the prior two procedures on the list. Arthrotomy or arthroplasty are both considered open-joint surgery. During this procedure, the surgeon makes an incision to visualize the TMJ and can then perform several different treatments to correct issues with the TMJ such as removal of growths, disc surgery, or recontouring the head of the jaw.
Joint replacement
For patients with severe degeneration of the TMJ, the entire joint can be replaced. This approach is generally rare and intended for people who have severe pain or extremely limited function.
Surgeries of the Jaw
Although this article is about TMJ surgery, it’s important to understand that many symptoms of TMJ disorder are not caused by the TMJs. Oftentimes an associated structure is contributing.
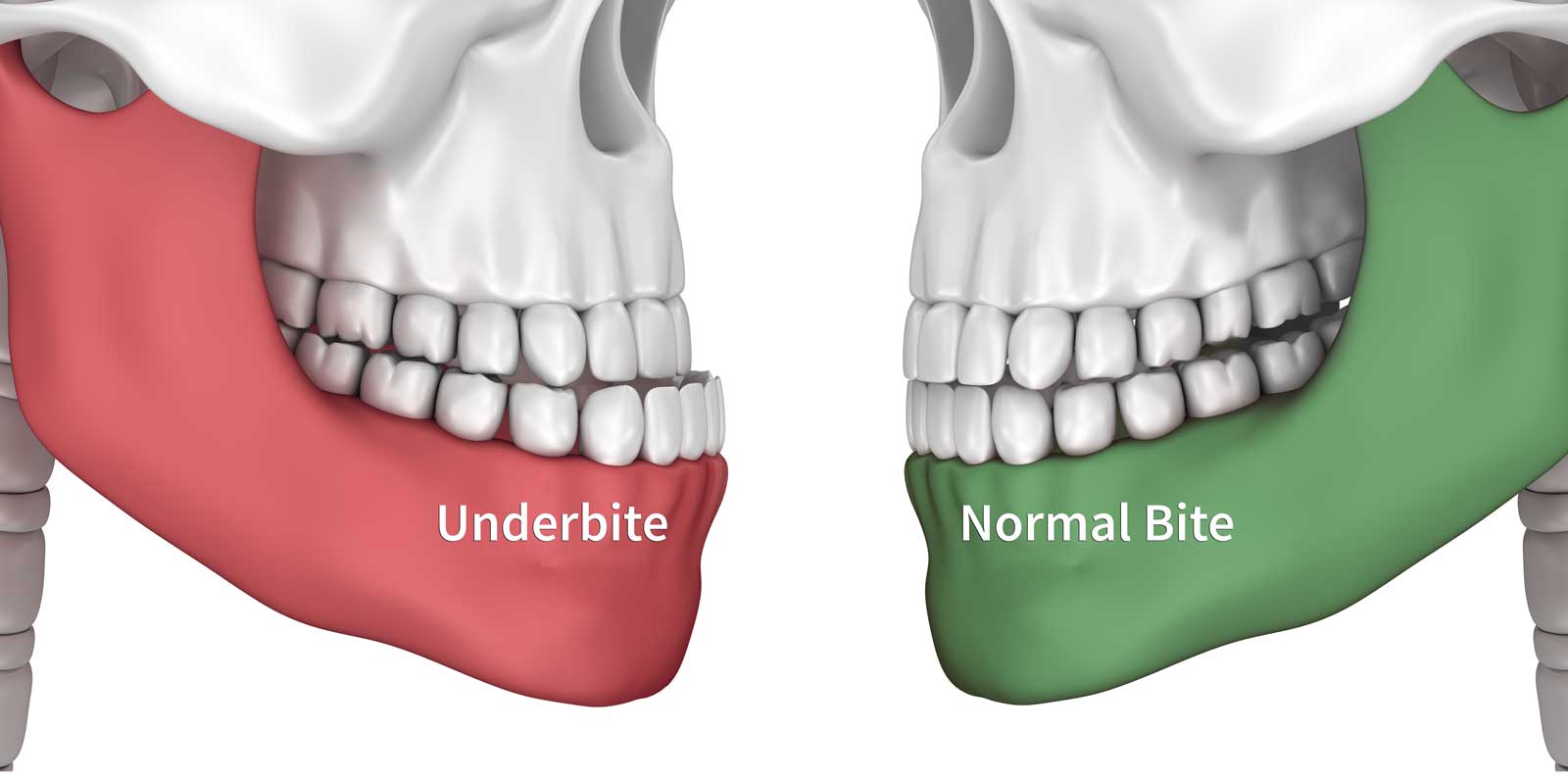
For example, you’ve probably heard the term overbite before. Overbite refers to how the top and bottom jaw orient to one another. If the top and bottom jaw are significantly malpositioned to one another, do you think it would create a strain on the TMJs when you open and close?
You bet it does.
So often what happens is, instead of doing TMJ surgery, the patient often first considers orthodontics to improve the alignment of the top and bottom jaws.
Lefort surgery or a bilateral sagittal split osteotomy (BSSO)
In some severe cases the top and bottom jaw are too far apart to align without surgery. In these cases, your healthcare provider may recommend a Lefort surgery or a bilateral sagittal split osteotomy (BSSO). Both these surgeries are methods that help the jaws to orient better to one another. They are surgeries of the top or bottom jaw, not the TMJ, however, these procedures significantly improve TMJ disorders when there are severe jaw misalignments.
How long is recovery?
Recovery from a TMJ surgery can vary dramatically depending on the type and complexity of surgery needed.
Arthrocentesis/arthroscopy generally heal in a few days, and Arthrotomy or arthroplasty heal in about two weeks. The more invasive procedures such as open surgery and BSSO can require 6-8 weeks of healing time.
Most TMJ surgeries, however, are completed as outpatient procedures, which means you’ll be able to go home the same day as the surgery.
After TMJ surgery, the biggest focus is on rest. The area needs a significant amount of rest to heal properly without placing significant tension on the jaw. During the time of rest after TMJ surgery, there is also quite a routine to follow to help you heal easily. Some common recommendations after TMJ surgery are:
- Take antibiotics, pain medication, and anti-inflammatory drugs as recommended by your healthcare provider.
- Stay hydrated and maintain a limited diet of soft foods.
- Apply a cold compress to the area to help with swelling the first day of surgery, and then switch to warm compresses,
- Cover up any bandages before bathing or showering.
- Regularly remove and replace bandages typically with antibiotic ointments if your healthcare provider recommends it
- In some cases, your jaw may be fixed in a position to heal, similar to a cast, or you may be asked to wear a splint to guide healing.
See your healthcare provider for follow-ups as they request over the first 6-12 weeks of healing.
Your healthcare provider may also request you to see a physical therapist to rehabilitate proper motion in your jaw after healing.
What TMJ Surgery Risks and What’s the Success Rate?
You probably notice a theme in my writing that I’m a big advocate to try all other options available before considering TMJ surgery.
The reason is because there are some notable risks to the procedure. The most common complications of TMJ surgery are a permanent loss in the range of motion and failure for the procedure to help the symptoms of TMJ. That’s devastating. And although in some rare cases TMJ surgery truly is the best option, it’s usually best to try other options first because there is a chance the surgery can be unsuccessful.
Other possible complications of TMJ surgery include:
- injury of nerves that could affect sensation or movement of the face
- damage to nearby structures
- infections in the short term after surgery
- persistent pain
- limited range of motion
- damage to the parotid gland
So what’s the success rate of TMJ surgery?
Well, it depends on the type of TMJ surgery and the complexity of the symptoms being treated. However, a study found an 83% success rate for arthroscopic surgery. Another study that looked at patients who underwent open joint surgery found a total of 22 patients (71%) reported improvement in pain score and 19 (61%) reported an improvement in mouth opening 12 months postoperatively.
It’s also important to understand that for TMJ treatment, success is judged as an improvement of symptoms. Patients that achieve an incremental improvement of symptoms often are considered a successful result.
It is often unrealistic for a complete resolution of all TMJ symptoms for severe patients, but often many patients find successful relief with a large proportion of their symptoms resolved.
The Bottom Line
Talk with your dentist early to diagnose if you have worsening TMJ issues. He or she may have suggestions for you. Alternatively, they may choose to refer you to a TMJ specialist.
It’s much easier to treat TMJ disorder early. Typically people that require surgery as a TMJ treatment have a severe progression of the condition or they have a congenital issue.
The key to understand is that many TMJ issues can be successfully treated without TMJ surgery if addressed earlier in progression.