TMJ TREATMENT IS LIBERATING
TMJ pain can be a huge limitation on your life. Many patients suffer for far too long because the symptoms are confusing–often vague and diffuse.
Unburden yourself from TMJ pain. We are a TMJ dentist in metro Boston. We’ll help you every step of the way.
LIVING AGAIN
Studies show that 70% of the world population have at least one symptom of temporomandibular joint (TMJ) disorder and 12% of the population suffer with severe TMJ symptoms everyday.
You are not alone. TMJ symptoms most commonly present as soreness upon biting, headaches, or jaw discomfort. Symptoms usually are created by a lack of harmony between the patient’s bite, muscles, and/or temporomandibular joint which is simply called TMJ for short. When the harmony of these structures is treated, balance is created and the TMJ symptoms improve.
Our Commitment
“I was fortunate to recognize the rise in TMJ dysfunction very early in my career. I sought direct mentorship from two of the founding fathers of the specialty of TMJ, Dr. Jeffery Okeson and Dr. Robert Kerstein. This unique background solidified my passion for TMJ treatment and catapulted my career as a nationally leading expert. For this, I am forever thankful.”
Dr. Charles Sutera
So What is this “TMJ” Temporomandibular Joint Disorder Thing?
As anyone looking into the topic probably notices, understanding TMJ is very convoluted. Even the name is disputed. Is it properly called TMD or TMJ? At Aesthetic Smile Reconstruction, we try to make the process simple to understand. Although there are many different philosophies and opinions, our practice takes a comprehensive approach which encompasses all the leading philosophies and treatments.
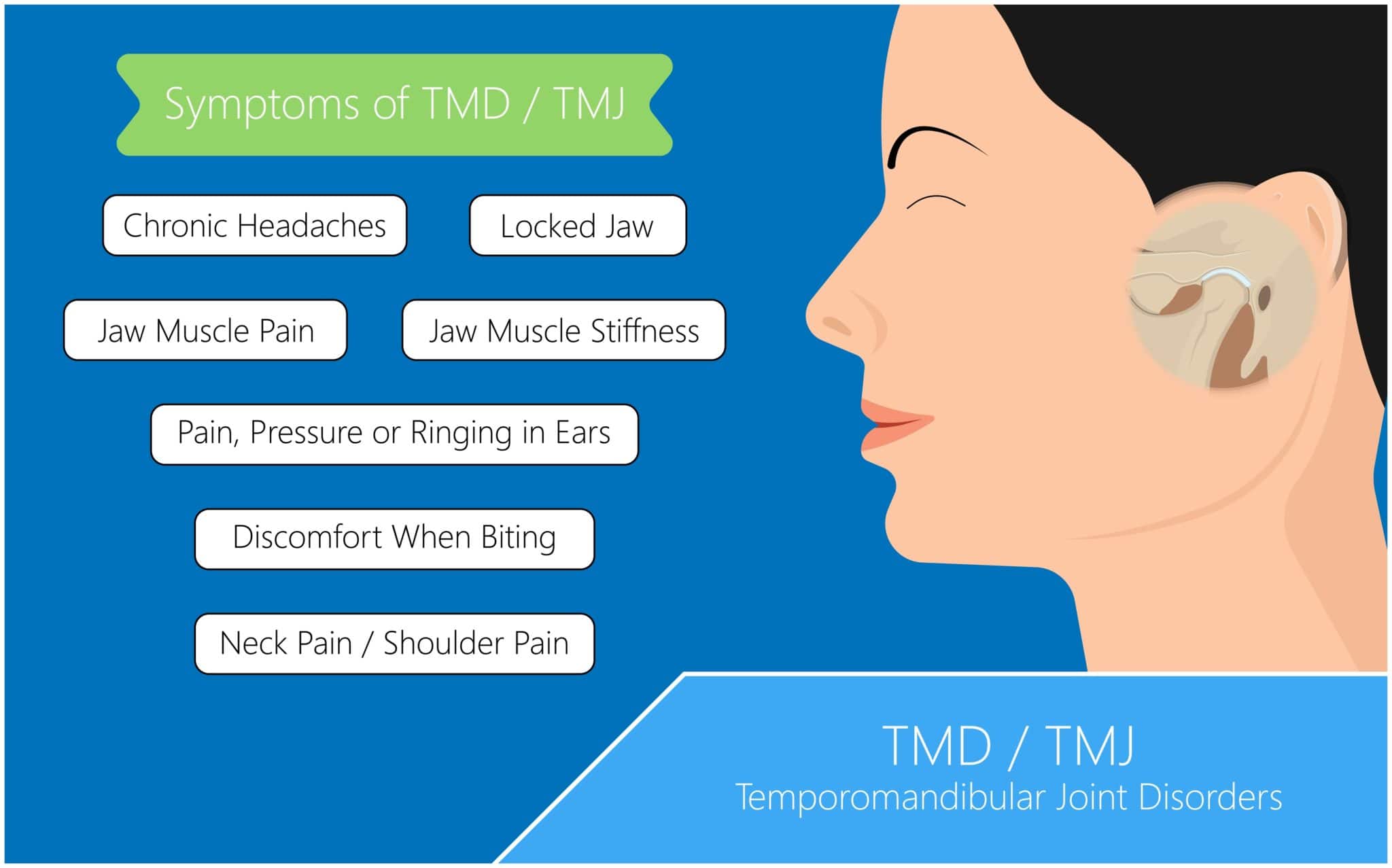
Symptoms usually are created by a lack of harmony between the patient’s bite, muscles, and/or temporal mandibular joint. For example, if the position of the teeth puts strain on the temporal mandibular joint or the muscles around it, over time the strain causes pain.
It may sound overwhelming, but it really isn’t as complicated as it may seem. It is best to understand TMD as a continuum based on two criteria. The first is the degree a patient is out of TMJ harmony. The second criteria is how long have the symptoms been left untreated. These two criteria will dictate the treatment needed and will also dictate the amount of improvement that is reasonably achievable.
Studies show more people live with chronic pain than cancer, heart disease and diabetes–combined!
Treating TMJ pain early is important for overall well being. It can be distracting to have chronic pain…all the time.
What are common Options for TMJ Treatment?
The first step in reviewing a patient with TMJ symptoms is simply getting to know them. Dr. Sutera will obtain a sense of contributing factors from the patient’s lifestyle, work environment, prior trauma, and personality type. This not only builds rapport, but also helps to discuss any additional factors which could be linked to exacerbating the patient’s symptoms. A comprehensive exam of the head and neck is completed. Factors that are examined are tenderness muscles, joint mobility, how the teeth come together, the position of the top and bottom jaw relative to one another, and contributing factors like headaches or ear pain.
After examination a treatment plan is created and discussed with the patient. Some treatment options that may be a part of the plan may include the following.
Orthotic / Occlusal Splint

A customized orthotic appliance repositions the jaw into a more stable position. Just like a cast for a broken bone, the stable position allows the muscles and joints of the jaw to heal.
Occlusal Equilibration

The teeth are designed to fit together in a particular balanced way. In many cases the teeth hit harder in some spots than others. This uneven force can be like trying to run in a stilleto high heal. The muscles feel strained by the instability. By balancing the teeth with a device called a T-scan, symptoms can improve.
Orthodontics

The alignment of how the top and bottom jaw come together can create tension on the muscles and joints of the jaw. Orthodontics like clear aligners can allow for a more harmonious position to remove the tension.
Restorative Dentistry

Severely worn or broken teeth create unbalanced force muscles and TMJ of the jaw. To balance the force, the teeth can be restored with dental crowns, bridges, implants, or composite fillings which reduce symptoms.
Botox
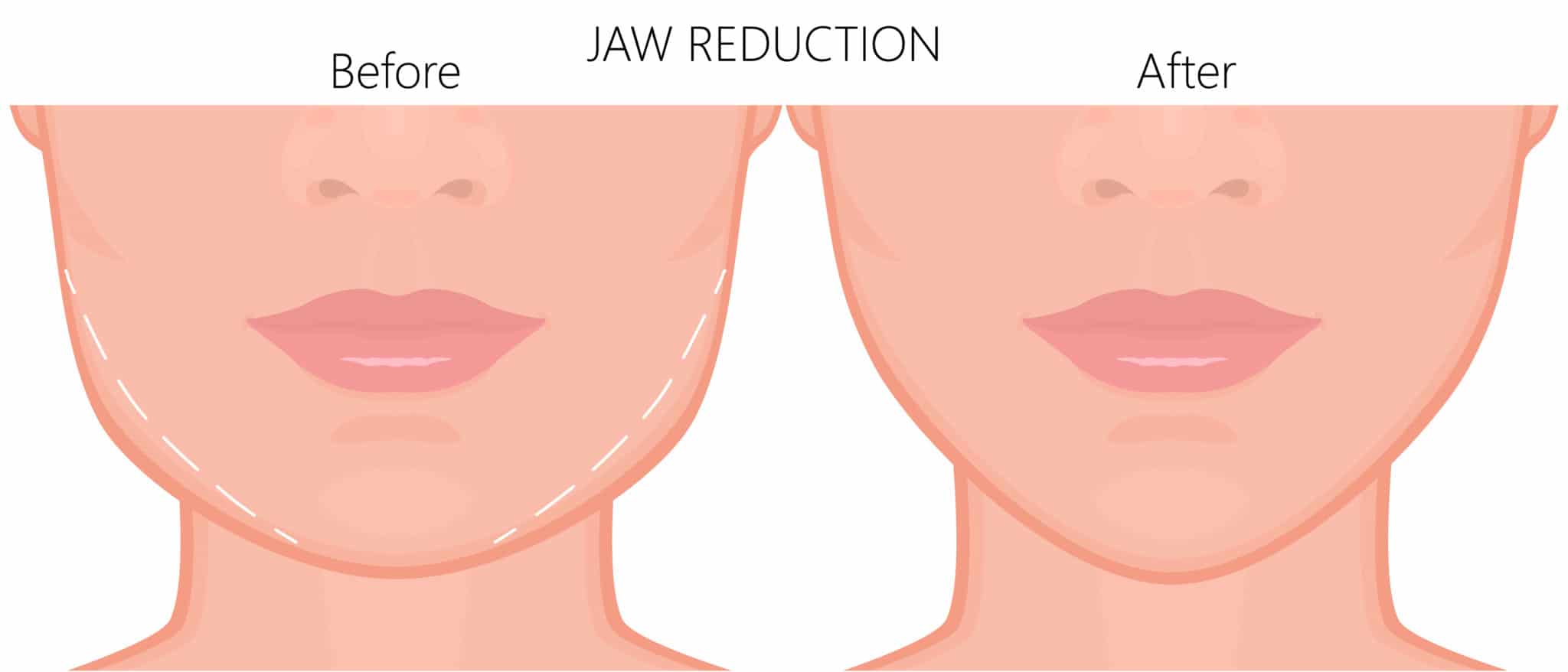
The muscles play a huge rule in the pain of TMJ disorder. When the muscles are overly powerful, the joints are overloaded with force. Botox can help assist the muscles to relax and reduce load on the entire TMJ complex.

